FAQ: Why do I need to enter ICD-10 Diagnosis codes into NextGen® Inpatient Clinicals (NGC) and other NextGen® applications, such as NextGen® Inpatient Financials (NGF)?
Answer: Although some codes do pass between applications (such as the Admitting Diagnosis from NGF to NGC), there may be times when the codes entered into a NextGen Healthcare application do not pass to another application. Due to the constraints of the interfaces between applications, some diagnosis codes will need to be re-entered into NextGen Inpatient Clinicals.
While all financial and reimbursement reporting will be completed out of the Financials application, there are many reports within NGC that calculate based on the patient’s ICD-10 code. If those codes are not properly recorded within NGC, the reports will not calculate properly.
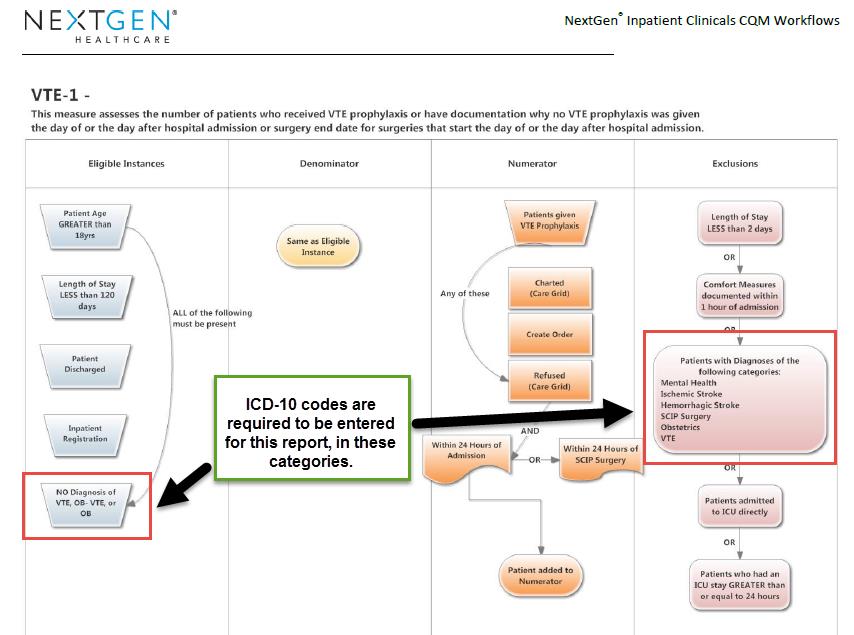
For example, all facilities should be submitting the 2012 CQM (Clinical Quality Measure) reports. Using the VTE-1 2012 CQM report as an example, the patient will be included as an eligible instance if he has NO recorded diagnosis of VTE, OB-VTE or OB. Additionally, any patients who have a diagnosis of a mental health condition, ischemic or hemorrhagic stroke, or SCIP surgery will be excluded from the report.
The diagnosis codes that the system is “looking for” have been built into the application (“hardcoded”), and will calculate automatically. If the facility does not confirm that the correct codes are entered, the patient may be erroneously included or excluded from the reports.
Although this is only one report example, many of the reports with NGC calculate in the same manner. For this reason, it is vital that all facilities ensure that all ICD-10 codes are entered into NGC. Although this process has not changed since the ICD-10 compliance date, many users are only now recognizing the importance of completing this step.
If this process is new to your facility, NextGen Healthcare recommends implementing a policy and procedure which outlines when the codes will be entered, and by whom. It is acceptable to have the facility’s coders enter the codes into NGC, as they are entering them into NGF. This can often be the best method to ensure that the patient has the same codes entered into all applications.