The process for maintaining the code sets for ICD-9, ICD-10 and CPT codes has been refined with the NextGen® Inpatient Clinicals v2.6.7 release, which is now available. With these updates, when a procedure/service is setup to check medical necessity checking, the ICD-10/ABN Medical Necessity checking will be supported at the ICD-10 Compliance date of October 1, 2015.
ICD-9/ABN Medical Necessity checking will be supported; however, if a CPT code has been retired, the facility must ensure the Charge Definition and Service data for Advance Beneficiary Notice (ABN) checking is setup correctly.
Facilities must ensure that retired codes are removed and updated codes set in the Charge Definition and Service data, in order for ABN checking to function correctly.
There are four parameters that must be set for the system to check medical necessity for a service:
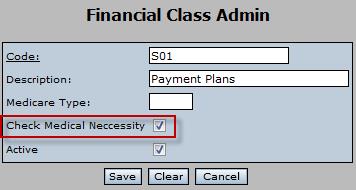
- The Check Medical Necessity check box must be enabled (checked) for the patient financial class in Financial Class Admin.
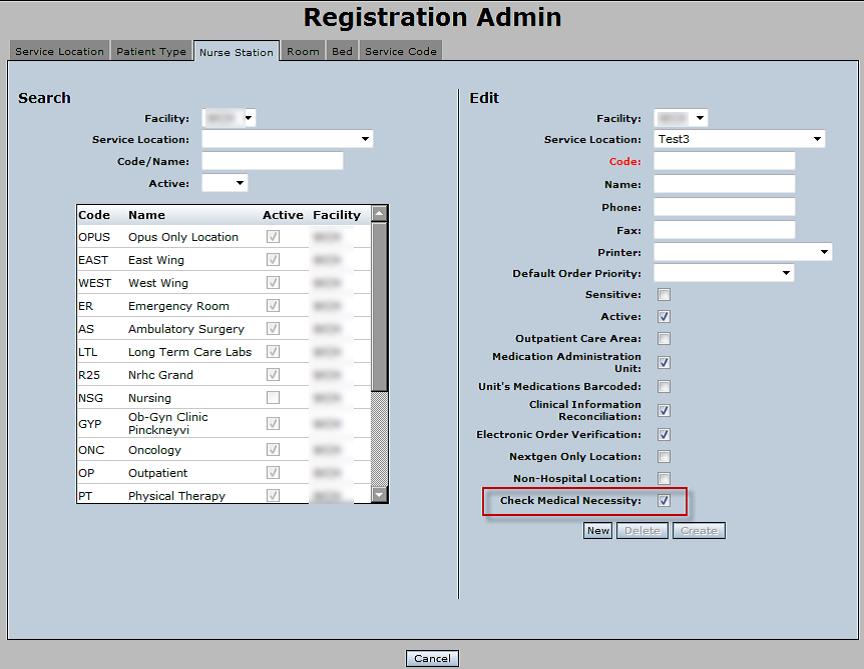
- The Check Medical Necessity check box must be enabled (checked) for the patient location in Registration Admin.
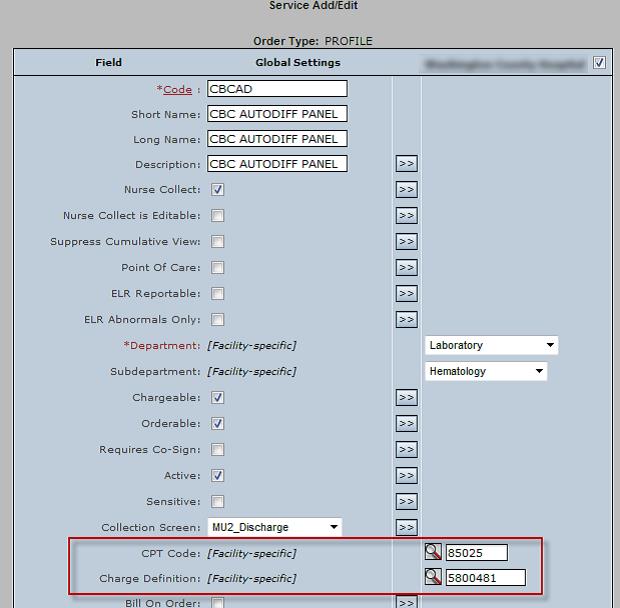
- The appropriate CPT Code must be assigned for the facility service in the Charge Definition.

- The Orderable check box must be enabled (checked) for the service in Service Add/Edit. The CPT Code and Charge Definition fields must also be set and correspond to the codes set in the Charge Definition for the service.
As part of the 2.6.7 upgrade, the Technical Support team will include the list of retired CPT codes as determined during your upgrade.
If your facility performs “Charge on Chart” through KBM, these CPT codes must also be assessed. Contact HospitalSupport@NextGen.com for assistance.
