The “2-Midnight Rule”, put forth by the Centers for Medicare & Medicaid Services (CMS), requires an inpatient hospital stay to be at least two or more midnights in order for the stay to be deemed as a medically appropriate inpatient admission. (CMS Part A payment is usually suitable in this case.) If the provider determines the patient’s care will not require a stay consisting of at least two midnights, and it is acceptable to treat the patient in an outpatient status, Part A payment is normally inappropriate. (In the cases, where the provider is unsure of the patient’s future needs, the patient may be placed in observation and an inpatient order placed for the patient at a later time).
To meet these requirements, documentation in the patient’s medical record, stating the need for the length of stay, must be fully and clearly recorded. NextGen® Inpatient Clinicals aims to ease the documentation process by incorporating additional information screens, for capturing specific patient data at the point of order entry.
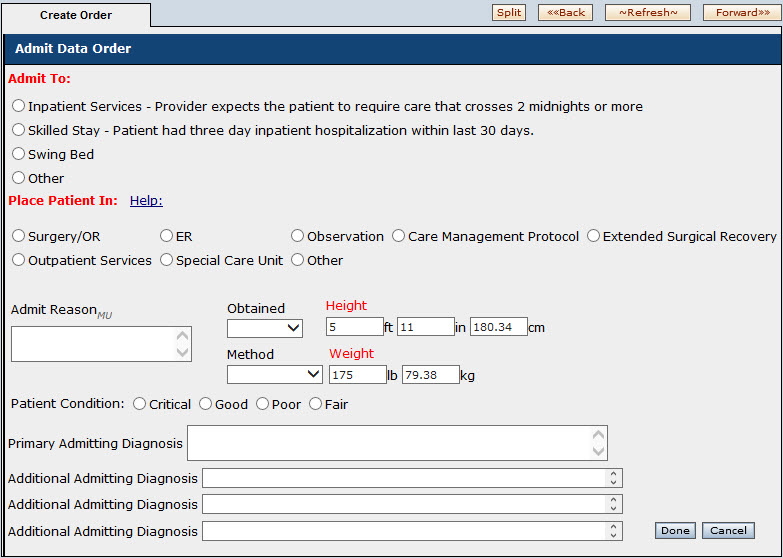
NextGen® Inpatient Clinicals Knowledge Base Model (KBM) v2.0.2 contains the following collection screen. (Accessed by clicking on the Red Icon, when creating an Admit order, from within the Create Order tab.)
The following updates to this screen became available in NextGen Inpatient Clinicals KBM v2.0.3 (in General Release as of 09/02/2014):
Significant changes to this collection screen include:
-Removal of the “Help” box and additional information on patient level selection. This provides a clinician additional information for patient acuity determination, with reduced button clicks. Under “Inpatient Services”, a clear definition of the “2-Midnight Rule” is included.
-Redesign of the screen. The screen is now easier to read and navigate, due to streamlining of the organization and layout.
-Height and Weight is no longer available. It has been determined there is no need to include this extra information since it is captured and available in many other areas throughout the chart.
-Primary Admitting Diagnosis is now a required field.
Currently, inpatient Part A claims only report the time the patient spent as an inpatient, and not the outpatient time spent in the facility. If a patient remains in the inpatient setting for fewer than two midnights (due to an unforeseen circumstance, such as death, transfer, improvement or departure against medical advice), this must also be properly documented. Other unusual circumstances may exist. For more detailed information on the benchmark 2-Midnight Rule, please review the below websites:
http://www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/Medicare-FFS-Compliance-Programs/Medical-Review/InpatientHospitalReviews.html http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/Downloads/SE1333.pdf http://cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/Medical-Review/Downloads/QAsforWebsitePosting_110413-v2-CLEAN.pdf