Our Authorized Certification Body (ACB) the Drummond Group, recently notified NextGen Healthcare that certification criteria 170.315(g.2) has been updated is in accordance with the Quality Payment Program (QPP) 2018 Final Rule (82 FR 53568) as pertains to the definition of “timely access” as required by the MIPS Promoting Interoperability (PI) transition measure for Patient Electronic Access.
Previous QPP rulings and related certification requirements left the definition of timely access as unspecified. With this latest change, both the MIPS PI transition and Medicaid PI modified Stage 2 measures require providers to give patients timely access within 4 business days of the encounter. (Note: MIPS PI non-transition and Medicaid PI Stage 3 still define timely access as occurring within 48 hours of the encounter.)
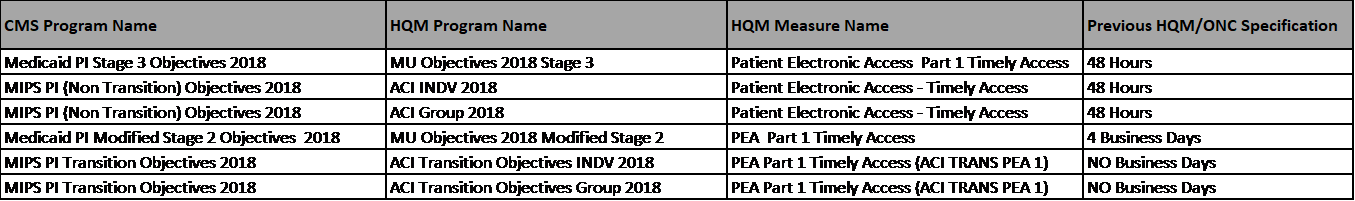
Due to the previously inconsistent definition of timely access across the various CMS programs, NextGen Healthcare maintained both versions of the measure on the Health Quality Measure (HQM) portal.
As of October 25, the Patient Electronic Access measure was updated for all programs on the HQM portal to align with updated regulatory requirements (see below table).
NextGen Healthcare anticipates that clients who are reporting the 2018 MIPS PI Transition measures will be most directly impacted by this update, particularly if they have not enabled PHR in System Administration. Clients unfamiliar with this configuration and who require assistance should contact Support to open a case. The above changes were part of the 10/25/2018 release of HQM.
